Preventing and managing chronic conditions – such as inflammatory bowel disease (IBD) and irritable bowel syndrome (IBS) – is a key challenge for health systems across Canada. Many patients who are at risk of developing IBD/IBS or other chronic conditions are not proactively identified and engaged to reduce their risk of developing the condition, or to support intervening at an early stage in the hopes of minimizing its negative impacts. Implementing a PHM approach to support the prevention and management of chronic conditions is promising in that it can drive the process of identifying those most in need, designing person-centred care models and monitoring and evaluating progress to inform learning and improvement efforts. PHM approaches are ideally integrated into a continuum of care with a strong grounding in primary care, however, there haven’t been attempts to define and synthesize what is known from best evidence about the optimal models for linking primary-care based PHM approaches with specialty service lines.
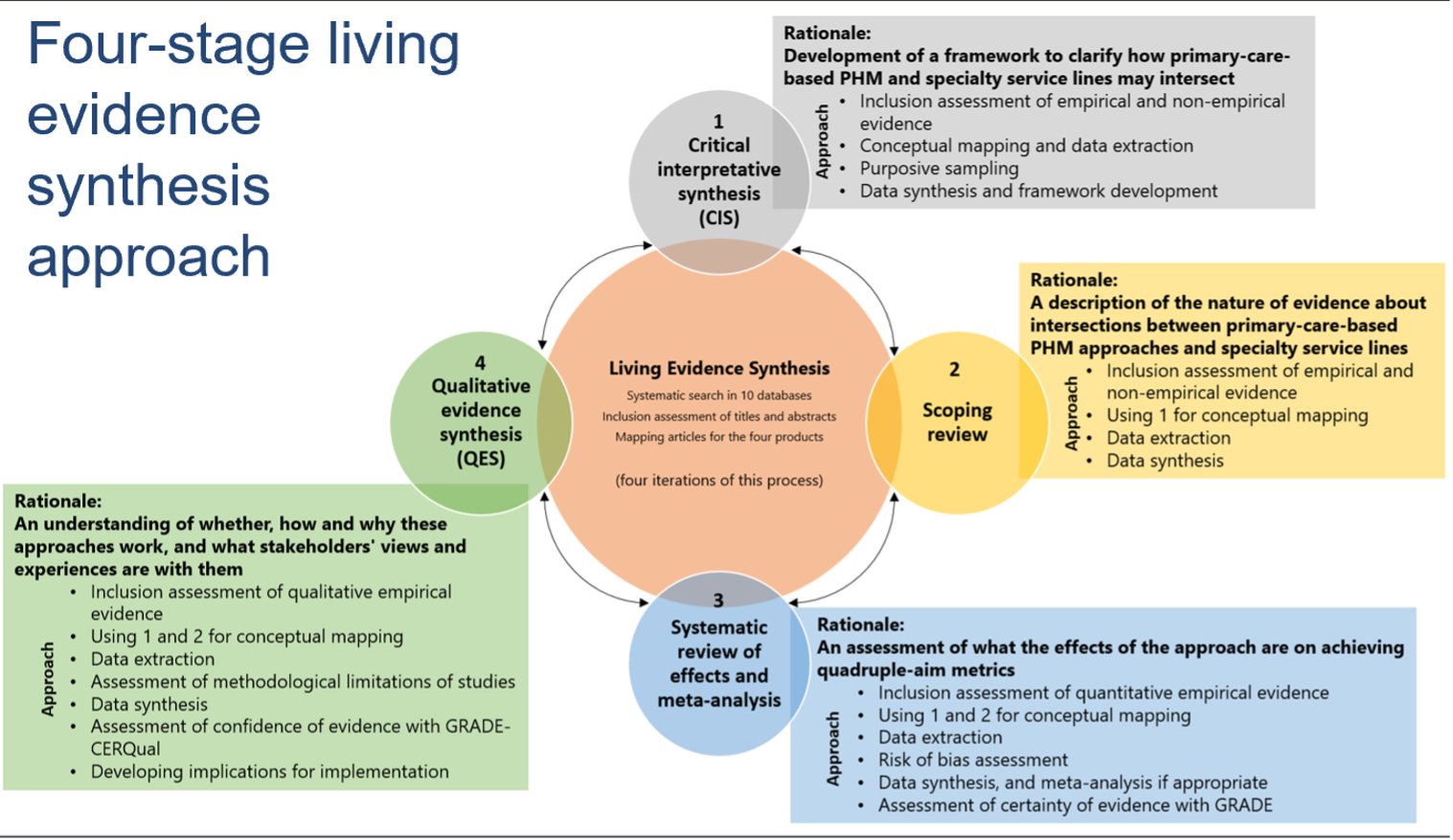
To address this challenge, we created a working group of system and organizational leaders, professional and patient leaders, as well as research leaders from the IMAGINE network to help oversee the design and implementation of a cutting-edge approach to evidence syntheses – a multiphase ‘living’ evidence synthesis – that will regularly synthesize empirical and non-empirical evidence about how to optimize the intersections between primary-care based PHM approaches and specialty service lines.
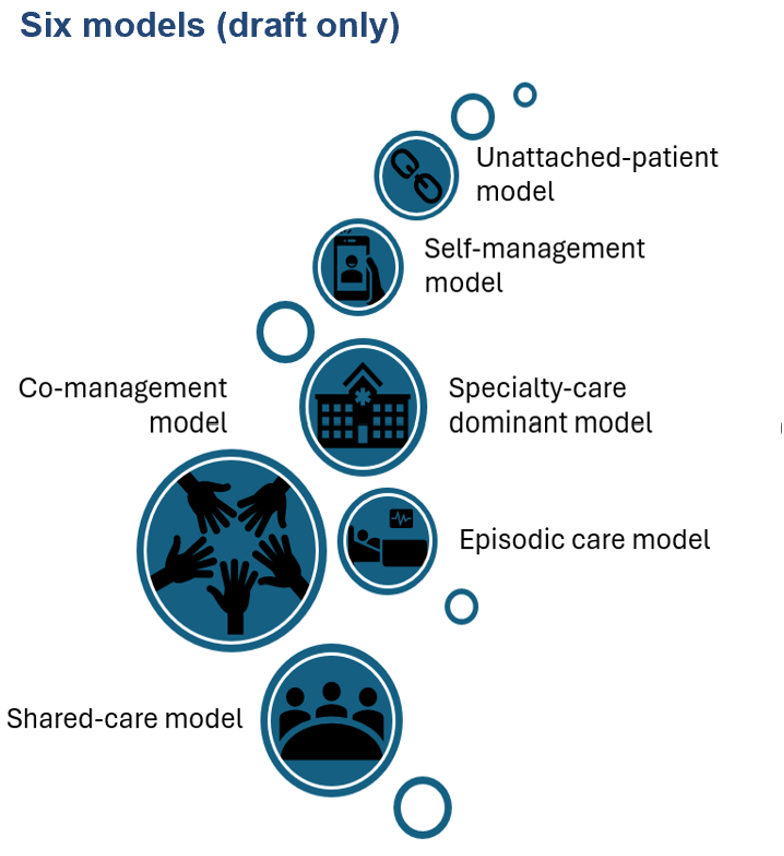
The working group consists of seven patient partners with lived experience with IBD/IBS and seven organizational, system or professional leaders (all of whom were also researchers focused on IBD/IBS or health systems and primary care). Over six meetings between October 2023 and September 2024, the group oversaw the development of a protocol for a four-stage living evidence synthesis and the completion of its first phase: which resulted in development of a framework that identified six models of care that can be used to understand and plan for optimizing efforts to link (see draft figures below). The group will continue to meet quarterly to advance stages 2-4 in the coming months and refine the outputs of stage 1 (including the models of care).
In the short term, the models identified through the work will influence how we structure our synthesis of empirical and non-empirical evidence in the next stages of our work, where we aim to establish what we know about the benefits (and potential harms) of each approach, what it means for patients and professionals managing IBD/IBS, and for system and organizational leaders. In the medium term, this work will also be used to inform the work at least one other SPOR Network (Chronic Pain Network), and we anticipate that it will be useful in supporting the work of the full range of SPOR Networks focused on chronic disease and on primary care. For example, the models of care can be adapted and contextualized (e.g., through complementary evidence syntheses products, or by adding additional stages to this existing living evidence synthesis) for use across a range of chronic conditions. Over the long term, we anticipate the outputs of this work will prove helpful in structuring ongoing evidence-informed conversations across Canadian health systems about how a primary-care based PHM approach can be used to establish chronic disease prevention and management systems – and specifically how to forge stronger linkages across primary care and specialty service lines.
